According to The Department of Health, the new Serious Incident Response Scheme (SIRS) commenced 1 April 2021. Under this scheme, residential aged care providers must notify the Aged Care Quality and Safety Commission (ACQSC) whenever certain “reportable incidents” occur. Today we look at what is and isn’t a “reportable incident.”
For a general summary of the SIRS see our previous article: Serious Incident Response Scheme (SIRS): A Summary for Residential Aged Care Providers.
For a closer look at some of the important questions raised by the SIRS, see our previous article: Serious Incident Response Scheme (SIRS): FAQs for Residential Aged Care Providers.
What is the Serious Incident Response Scheme (SIRS)?
The SIRS is a national framework for incident management and reporting of serious incidents in residential aged care. It imposes obligations on aged care providers to manage and report on incidents, and expands the powers of the Aged Care Quality and Safety Commission (ACQSC).
SIRS Reporting Requirements
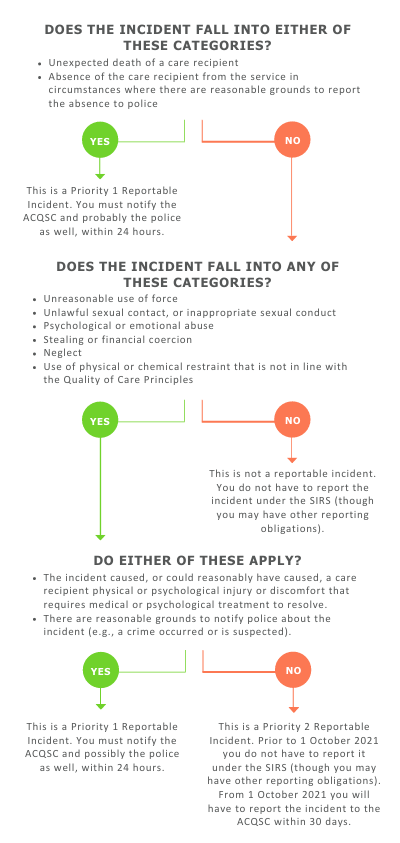
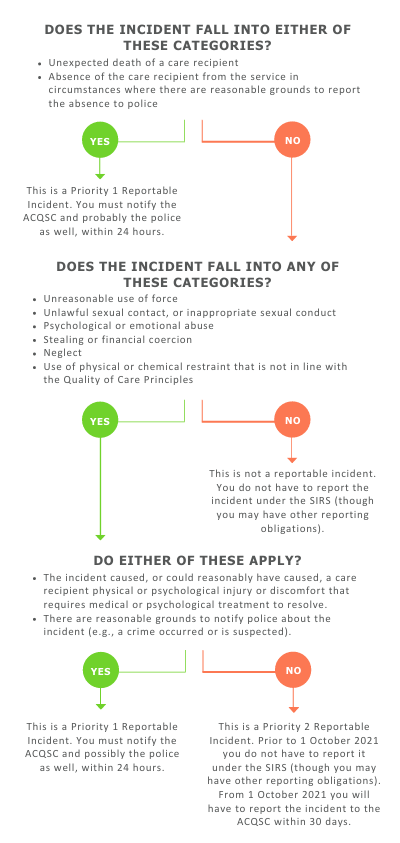
From 1 April 2021, you must notify the ACQSC of every “Priority 1 reportable incident” within 24 hours of becoming aware of the incident. To be clear, you do not have to notify the ACQSC of every incident. You only have to notify the ACQSC of an incident that is classified as a “reportable incident” AND “Priority 1.” This means you need to understand:
- What is a “reportable incident”?
- Which reportable incidents are “Priority 1”?
(Note: from 1 October 2021, you will also have to report all “Priority 2” reportable incidents. We will cover this requirement in detail later this year.)
What Is and Isn’t a “Reportable Incident”?
According to the SIRS, “A reportable incident is any of the following incidents that have occurred, are alleged to have occurred, or are suspected of having occurred, in connection with the provision of residential care, or flexible care provided in a residential setting, to a residential care recipient of an approved provider”:
- unreasonable use of force against the residential care recipient
- unlawful sexual contact, or inappropriate sexual conduct, inflicted on the residential care recipient
- psychological or emotional abuse of the residential care recipient
- unexpected death of the residential care recipient
- stealing from, or financial coercion of, the residential care recipient by a staff member of the provider
- neglect of the residential care recipient
- use of physical restraint or chemical restraint in relation to the residential care recipient (other than in circumstances set out in the Quality of Care Principles)
- unexplained absence of the residential care recipient from the residential care services of the provider.
Before we look at each of these in detail let’s note a general rule about what is not a reportable incident.
Incidents resulting from a care recipient’s refusal to receive care are not “reportable incidents”
The SIRS says that the incidents listed above are not reportable if “the incident results from the residential care recipient deciding to refuse to receive care or services offered by the approved provider.” In practice, this exception would apply only in very limited situations. Now let’s look closely at each of the “reportable incidents.”
Unreasonable use of force against the residential care recipient
Includes: “conduct ranging from a deliberate and violent physical attack to use of unwarranted physical force.” E.g., hitting, pushing, shoving, or rough handling.
Does not include: gently touching the residential care recipient for the purposes of providing care, attracting attention, guiding or comforting.
Unlawful sexual contact, or inappropriate sexual conduct, inflicted on the residential care recipient
Includes:
- any non‑consensual contact or conduct of a sexual nature, e.g, sexual assault, acts of indecency and the sharing of an intimate image of the residential care recipient
- conduct done with the intention of making it easier to get the residential care recipient to engage in sexual contact or conduct
- conduct or contact by a care provider (staff or volunteer) that is of a sexual nature. This conduct must be reported even if it is consensual
- conduct or contact by a care provider (staff or volunteer) that involves any touching of the care recipient’s genital area, anal area or breast in circumstances where this is not necessary to provide care. This conduct must be reported even if it is consensual.
Does not include: consensual contact or conduct of a sexual nature between the residential care recipient and a person who is not a staff member of the approved provider (e.g., another resident).
Psychological or emotional abuse of the residential care recipient
Includes:
- conduct that has caused the residential care recipient psychological or emotional distress
- conduct that could reasonably have been expected to have caused a residential care recipient psychological or emotional distress
- taunting, bullying, harassment or intimidation, threats of maltreatment, humiliation
- unreasonable refusal to interact with the residential care recipient or acknowledge the recipient’s presence
- unreasonable restriction of the residential care recipient’s ability to engage socially or otherwise interact with people
- repetitive conduct or contact which does not constitute unreasonable use of force but the repetition of which:
- has caused the residential care recipient psychological or emotional distress; or
- could reasonably have been expected to have caused a residential care recipient psychological or emotional distress.
Unexpected death of the residential care recipient
Includes death in circumstances where:
- reasonable steps were not taken by the approved provider to prevent the death; or
- the death is a result of:
- care or services provided by the approved provider; or
- a failure of the approved provider to provide care or services.
E.g., death in the event of a fall, untreated pressure injury, or the actions of a consumer result in the death of another consumer.
Stealing from, or financial coercion of, the residential care recipient by a staff member of the provider
Includes:
- stealing from the residential care recipient by a staff member of the approved provider
- conduct by a staff member of the approved provider that:
- is coercive or deceptive in relation to the residential care recipient’s financial affairs; or
- unreasonably controls the financial affairs of the residential care recipient.
E.g., if a staff member coerces a consumer to change their will to their advantage, or steals valuables from the consumer.
Neglect of the residential care recipient
Includes:
- a breach of the duty of care owed by the approved provider, or a staff member of the provider, to the residential care recipient
- a gross breach of professional standards by a staff member of the approved provider in providing care or services to the residential care recipient.
E.g., withholding personal care, untreated wounds, or insufficient assistance during meals.
Use of physical restraint or chemical restraint in relation to the residential care recipient (other than in circumstances set out in the Quality of Care Principles)
All uses of physical and chemical restraint are reportable incidents unless the use complies with section 15F (for physical restraint) or 15G (for chemical restraint) of the Quality of Care Principles 2014 (Cth).
Both 15F and 15G say that restraint can only be used as a last resort and set many requirements for assessment and reporting.
Examples of non-compliant uses of restraint (which must be reported) include:
- physical or chemical restraint used without prior consent or without notifying the consumer’s representative as soon as practicable
- physical restraint used in a non-emergency situation
- issuing a drug to a consumer to influence their behaviour as a form of chemical restraint.
Unexplained absence of the residential care recipient from the residential care services of the provider
Includes an absence of the residential care recipient from the residential care services in circumstances where there are reasonable grounds to report the absence to police.
What is a “Priority 1” Incident?
Remember, until 1 October 2021, you only have to report under the SIRS if the incident is a “reportable incident” AND “Priority 1”. So what is “Priority 1”?
A Priority 1 incident is any reportable incident that is ALSO one of these:
- an incident that caused, or could reasonably have caused, a care recipient physical or psychological injury or discomfort that requires medical or psychological treatment to resolve
- any incident where there are reasonable grounds to notify police (e.g., where a crime occurred or is suspected)
- any unexplained absence from care where there are reasonable grounds to report the absence to police
- any unexpected death.
Note: After 1 October you will also have to notify the ACQSC within 30 days of any reportable incidents that are “Priority 2”. A Priority 2 incident is effectively any reportable incident that is not Priority 1. We will cover this in more detail later this year.
Do I Have to Make a SIRS Report?

Further Resources
ABOUT THE AUTHORS
Mark Bryan
Mark is a Legal Research Consultant at CompliSpace and the editor for ACE. Mark has worked as a Legal Policy Officer for the Commonwealth Attorney-General’s Department and the NSW Department of Justice. He also spent three years as lead editor for the private sessions narratives team at the Royal Commission into Institutional Responses to Child Sexual Abuse. Mark holds a bachelor’s degree in Arts/Law from the Australian National University with First Class Honours in Law, a Graduate Diploma in Writing from UTS and a Graduate Certificate in Film Directing from the Australian Film Television and Radio School.
Jenny Wang
Jenny is the Content Integration Team Leader at CompliSpace and a legal research assistant for the aged care team. She has a Bachelor of Science (Financial Mathematics and Statistics) and is currently completing her Bachelor of Laws at the University of Sydney.